Summary (TL;DR)
The doctor–patient relationship has transformed from ancient obedience to modern partnership. Once, doctors acted and patients complied. Today, patients arrive informed, clinicians focus on empathy and nuance, and AI is reshaping how conversations unfold. This blog traces the historical evolution of that relationship, illustrates it through Carolina Millon’s cancer journey, and looks ahead to a future of “partnership by design.” With AI amplifying understanding and accessibility, doctors may shift from knowledge gatekeepers to sense-makers, ensuring care remains empathetic, contextual, and human.
1. From Obedience to Dialogue: A Historical Sweep
Over 4,000 years ago in ancient Egypt, medicine was hierarchical and priestly. Knowledge was secret. Healing was directive. This is what Kaba & Sooriakumaran later described as the activity–passivity model: the doctor acts, the patient obeys.
Across history, the balance of power shifted slowly:
- Greek medicine introduced observation and rationalism, encouraging dialogue.
- Medieval Europe returned to mysticism and authority.
- The Enlightenment expanded patient rights, yet the biomedical model still placed doctors firmly in control.
It wasn’t until the mid-20th century that the mutual participation model gained traction — where doctors and patients share information, weigh options, and decide together.
go to: | Start | Top of This Section | End
2. Patient-Centred Care as Modern Good Practice
In Blog 2 of this series, we explored Mead & Bower’s (2000) Five Dimensions of Patient-Centred Care. These remain the benchmark of good practice:
- Biopsychosocial perspective — care considers biological, psychological, and social contexts.
- Patient-as-person — recognising the patient’s biography, values, and meaning of illness.
- Sharing power and responsibility — moving from paternalism toward mutual decision-making.
- Therapeutic alliance — building trust, empathy, and shared goals.
- Doctor-as-person — acknowledging the clinician’s own personality, values, and emotions.
Carolina Millon’s story (Blog 1) demonstrates how these dimensions can come alive in practice — particularly when AI supports clarity, reduces fear, and enables true participation.
go to: | Start | Top of This Section | End
3. Carolina’s Case in Context
Traditionally, Carolina’s biopsy results would have been explained only during a brief doctor-led consultation. Instead, she accessed plain-language explanations within minutes.
- This did not replace her doctors’ expertise.
- It reduced fear by demystifying jargon.
- It prepared her to ask sharper questions.
- It created parity: she met her doctors as an informed partner.
Carolina illustrates the wider trend: knowledge is no longer the exclusive domain of clinicians. Patients can arrive already equipped to collaborate. AI doesn’t supplant expertise — it redistributes understanding.
go to: | Start | Top of This Section | End
4. The Fastest Leap in History
For most of history, changes in the doctor–patient relationship occurred over decades or centuries. Today, the shift is accelerated by digital tools and AI in real time.
- Information once locked in textbooks is now at patients’ fingertips.
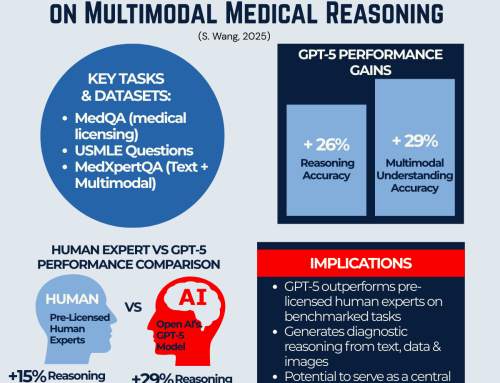
- Large language models (like GPT-5) can interpret medical data and explain it in plain language.
- Patients can explore “what if” scenarios — not to self-diagnose, but to engage more meaningfully in decision-making.
This is the fastest leap in history: from hierarchical to participatory medicine in a single generation.
go to: | Start | Top of This Section | End
5. Cultural and Global Implications
Not all systems evolve at the same pace. Paternalism remains dominant in many regions, where patients have limited access to data. AI, with its global accessibility, could flatten these hierarchies by making knowledge more universally available.
If a patient in São Paulo or Karainagar (a small island village in the far north of Srilanka) can access the same explanations and reasoning tools as a patient in Boston, the global playing field begins to shift. AI could become the great equaliser in health literacy.
6. Partnership by Design
The evolution from activity–passivity to AI-enabled mutual participation is not just about workflow. It is about redefining trust, power, and collaboration.
- Doctors remain essential experts, but their role evolves: from information gatekeepers to strategists, advocates, and sense-makers.
- Patients, equipped with knowledge, become active participants.
- AI acts as a bridge: clarifying, connecting, and equalising.
The result: better questions, better conversations, and better outcomes.
go to: | Start | Top of This Section | End
7. The Future: Super Agers and the Next Horizon
Here, the vision of clinicians like Eric Topol adds another layer. In his Super Agers work, Topol reframes aging around resilience and vitality rather than decline. AI is central to that transformation:
- Biomarkers and liquid biopsies can detect disease risk decades before symptoms appear.
- Wearables and sensors continuously capture real-time activity, heart rhythms, and sleep patterns.
- Genomics and organ clocks reveal a person’s true biological age, not just their chronological one.
No individual clinician can integrate all this information at scale. But AI can — turning torrents of data into precision prevention: personalised interventions, lifestyle prescriptions, and early warnings tailored to each patient.
This evolution reframes the doctor’s role yet again. In a world where AI manages data and prediction, doctors focus on sensing and context:
- Ensuring the right inputs are provided to AI.
- Validating AI outputs against the patient’s lived experience.
- Bringing empathy, trust, and nuance that no algorithm can replicate.
Seen through this lens, Carolina’s story is not just about interpreting biopsy results more clearly. It’s the first step in a broader transformation — where patients are empowered with knowledge, and clinicians are liberated to practice medicine as guides, advocates, and partners in health.
“AI will not replace doctors, but it will reshape their role: from gatekeepers of knowledge to sense-makers of care”
go to: | Start | Top of This Section | End
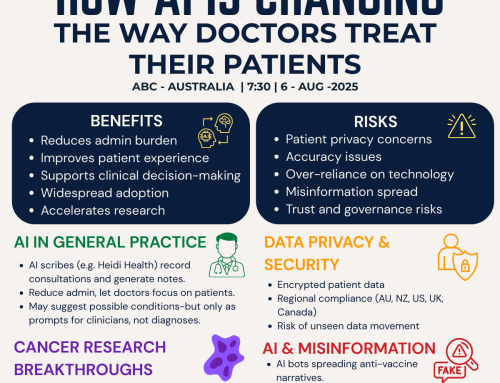
8. Implications for Practice & Leadership
For healthcare leaders and practitioners, this evolution raises urgent questions:
- How do we design systems that train both doctors and patients to collaborate with AI, not against it?
- How do we ensure AI enhances trust, not erodes it?
- What safeguards must be built for ethics, bias, and equity?
In workshops, we call this Partnership by Design: training clinicians and patients alike to see AI as a tool for shared decision-making. In blogs, it positions patient empowerment not as a sudden revolution, but as the culmination of centuries of gradual change — now accelerated by AI.
Conclusion: From Hierarchy to Shared Humanity
The story of the doctor–patient relationship is the story of healthcare itself: from hierarchy to dialogue, from obedience to partnership.
Today, AI is the catalyst. It is not replacing clinicians. It is enhancing collaboration, empowering patients, and enabling care that is more informed, empathetic, and truly patient-centred.
The opportunity is historic. If realised, it could move us from elderly to wellderly, from systems of treatment to ecosystems of health, from reactive sick care to proactive vitality.
The next horizon is here. Let’s step into it together.
go to: | Start | Top of This Section | End
Relevant Blogs in This Series
👉 If you’re ready to continue, Blog 4 explores how GPT-5 is breaking barriers in multimodal medical reasoning — and what this means for the future of decision support in healthcare.
Here are the other blogs in this series:
1️⃣ From Patients to Partners — How informed patients like Carolina Millon are reshaping care.
2️⃣ The Five Dimensions of Patient-Centred Care — A framework for what “good care” looks like in practice.
3️⃣ From Ancient Egypt to AI — The fastest leap in the doctor–patient relationship in history. (This Blog)
4️⃣ Breaking Barriers — How GPT-5 is advancing multimodal medical reasoning beyond human expertise.
5️⃣ From Patients to Partners — AI’s real-world impact on healthcare.
6️⃣ Understanding the Patient Journey — A new framework for communication in modern healthcare.
🌍 We hope this series serves as a mini masterclass for practitioners and healthcare innovators — helping to reimagine healthcare and shape it for the better.
Before you move on, we’d love to hear from you:
Looking back at the history of the doctor–patient relationship — from ancient obedience to modern partnership — where do you see AI taking us next?
Please scroll down and
💬 Share your perspective in the comments below.
go to: | Start | Top of This Section | End
Join the Movement
If this series of blogs has sparked your imagination about how healthcare delivery could be transformed — making it more accessible, affordable, and equitable while also reducing burnout among healthcare professionals — we invite you to connect with the Co-Create Care Movement.
This growing community brings together healthcare innovators, leaders, clinicians, and forward-thinkers who are exploring how AI can be used responsibly to empower patients, support clinicians, and improve outcomes.
Connect with Co-Create Care movement.
→ Facebook Group: Aligning for Excellence
→ Community Link – Meetup Discussions @ AI in Practice (Our Fortnightly Online forum for live discussions)
Together, we can shape a future where healthcare isn’t just sustainable—it’s remarkable.
go to: | Start | Top of This Section | End
Reference
Mead, N. and Bower, P. (2000). Patient-centredness: a conceptual framework and review of the empirical literature. Social Science & Medicine, [online] 51(7), pp.1087–1110. doi:https://doi.org/10.1016/s0277-9536(00)00098-8.(Accessed: 11 August 2025)
Kaba, R. and Sooriakumaran, P. (2007). The evolution of the doctor-patient relationship. International Journal of Surgery, [online] 5(1), pp.57–65. doi:https://doi.org/10.1016/j.ijsu.2006.01.005.(Accessed: 11 August 2025)
OpenAI (2024) Introducing GPT-5 [YouTube video]. Available at: https://www.youtube.com/live/0Uu_VJeVVfo?t=2075 (Accessed: 11 August 2025). Segment: 34:35–40:55.
go to: | Start | Top of This Section | End





Leave A Comment