Beyond the 60-30-10 Challenge: Rethinking Healthcare Performance and Transformation
Introduction
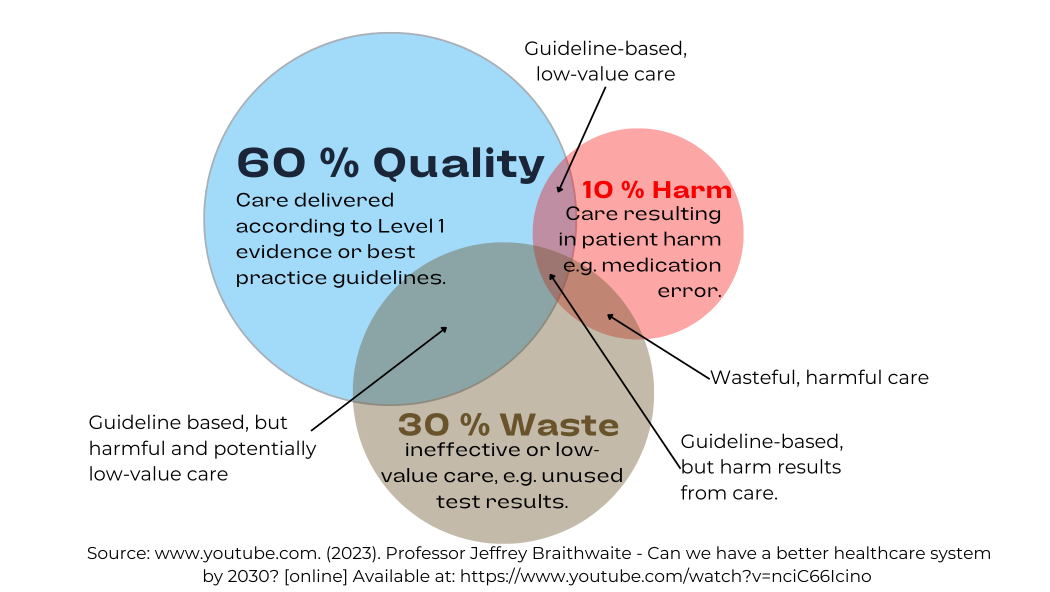
Despite continuous advancements in medical knowledge, technology, and policy changes, the healthcare system has remained trapped in a persistent cycle of inefficiency. The 60-30-10 Challenge, introduced by Braithwaite et al. (2020), starkly illustrates the stagnation in healthcare performance:
- 60% of care is evidence-based, aligning with clinical guidelines.
- 30% of healthcare spending is wasted on inefficiencies, redundancy, and unnecessary treatments.
- 10% of patients experience preventable harm, underscoring systemic failures in patient safety.
This article critically examines the key findings of Braithwaite et al.’s work, highlighting its central argument and assessing the feasibility of its proposed solutions.
go to: | Start | Top of This Section | End
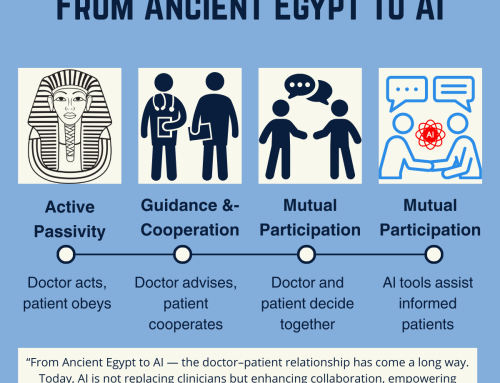
Why Healthcare is Stuck
Braithwaite et al. argue that the linear, command-and-control approaches used in healthcare management have failed to drive meaningful change. Traditional top-down policy interventions, bureaucratic mandates, and restructuring efforts have led to little improvement over the past three decades. The authors contend that these approaches ignore the complex, adaptive nature of healthcare systems, which require more dynamic and flexible solutions.
go to: | Start | Top of This Section | End
Critical Analysis: Strengths and Limitations
1. Strengths: A Well-Defined Problem and Systems-Based Approach
- Clarity of the 60-30-10 Framework: The authors successfully distil the inefficiencies of healthcare into three simple but powerful statistics, making the systemic challenges easily digestible.
- Acknowledgment of Complexity Science: The article moves beyond conventional thinking by positioning healthcare as a complex adaptive system, where interactions between different elements cannot be governed by rigid policies alone.
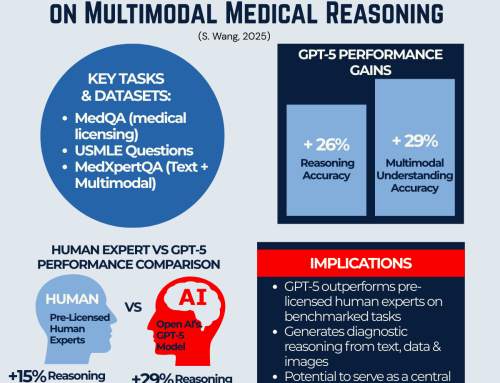
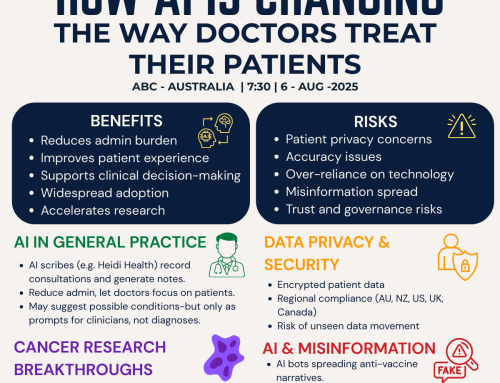
- Proposed Solution: The Learning Health System – The authors advocate for data-driven, continuously learning health systems that leverage AI, real-time analytics, and clinician-led adaptations to improve care.
2. Limitations: Challenges in Implementation
While the paper presents a compelling vision, several challenges remain unaddressed:
- Adoption Barriers: Many healthcare institutions are deeply entrenched in bureaucratic models, making it difficult to transition toward a learning-based system.
- Data Infrastructure and Interoperability: While the article emphasises the importance of real-time data and AI, it does not fully explore how fragmented health IT systems and regulatory constraints could slow down adoption.
- Human Resistance to Change: Healthcare professionals often resist externally imposed changes, especially if they perceive them as disruptive. The paper does not delve deeply into strategies to incentivize engagement from frontline clinicians.
go to: | Start | Top of This Section | End
The Future of Healthcare: Moving from Theory to Action
The learning health system model offers a promising alternative to the ineffective, compliance-driven healthcare models of the past. However, for real transformation, several factors must be considered:
- Empowering Clinicians and Localised Innovation: Change must come from within the system, leveraging the expertise of those delivering care rather than relying on external mandates.
- Aligning Incentives with Quality and Efficiency: Financial and operational incentives should reward better patient outcomes, not just higher volumes of care.
- Building Scalable Data Infrastructure: A national or global health data network would be necessary to implement AI-driven, real-time decision-making tools effectively.
- Encouraging Agile Policy-Making: Policymakers must shift from rigid regulations to flexible frameworks that support localized experimentation and adaptation.
go to: | Start | Top of This Section | End
Conclusion
Before we give our final thoughts, if this article or the article by Braithwaite et al. resonated with you, we invite you to join our community.
Join Our Community
The challenges outlined in this article demand a collaborative effort. If you’re passionate about transforming healthcare and want to be part of a forward-thinking network of professionals, innovators, and thought leaders, we invite you to join our community. Together, we can drive meaningful change, share best practices, and shape the future of healthcare.
Join our community today and be part of the movement toward a smarter, learning-based healthcare system.
Final Thoughts
The 60-30-10 Challenge is a wake-up call for the global healthcare system. Despite decades of policy-driven reforms, inefficiencies, waste, and patient harm persist at unacceptable levels. Braithwaite et al. rightly argue that a learning health system model—one that embraces data-driven insights, continuous improvement, and clinician-led change—offers a viable path forward. However, transitioning to this model will require overcoming cultural resistance, investing in interoperable data systems, and fostering an environment that supports adaptive learning.
The question remains: Will healthcare leaders take the bold steps necessary to move beyond the stagnation of the past three decades? Or will the system continue to cycle through ineffective top-down reforms? The time to act is now.
References
Braithwaite, J., Glasziou, P., & Westbrook, J. (2020). The 60-30-10 Challenge: Implementing evidence-based care, reducing waste, and improving patient safety. BMC Medicine, 18(1), 102. https://doi.org/10.1186/s12916-020-01563-4
Braithwaite, J. (2020). The 60-30-10 Challenge in Healthcare [YouTube video]. AIHI Webinar Series. Available at: https://www.youtube.com/watch?v=nciC66Icino [Accessed 18 Feb. 2025].
Please email your thoughts to [email protected] or scroll down and leave us a comment below.
go to: | Start | Top of This Section | End


Leave A Comment