Summary (TL;DR)
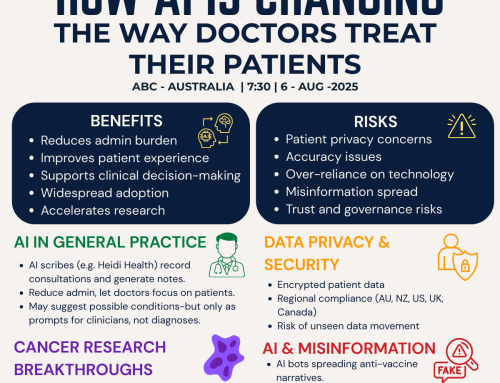
AI is creating information parity between patients and doctors, turning conversations into true partnerships involving smarter, more collaborative, and more informed conversations.
Building on the first four blogs in this series, this article shows how AI is creating information parity between patients and doctors. The result: smarter conversations, shared decisions, and true partnerships in care. The next article will reveal the Patient Journey Communications Framework. This new framework is a practical model for navigating these new dynamics.
Introduction: Connecting the Threads
This article brings together the insights of the first four blogs in this series.
- In Blog 1, we shared Carolina Millon’s story that demonstrated how she used AI to decode her biopsy report and step into her care as an informed partner.
- In Blog 2, we explored the Five Dimensions of patient-centred care and how Carolina’s journey reflected them in practice.
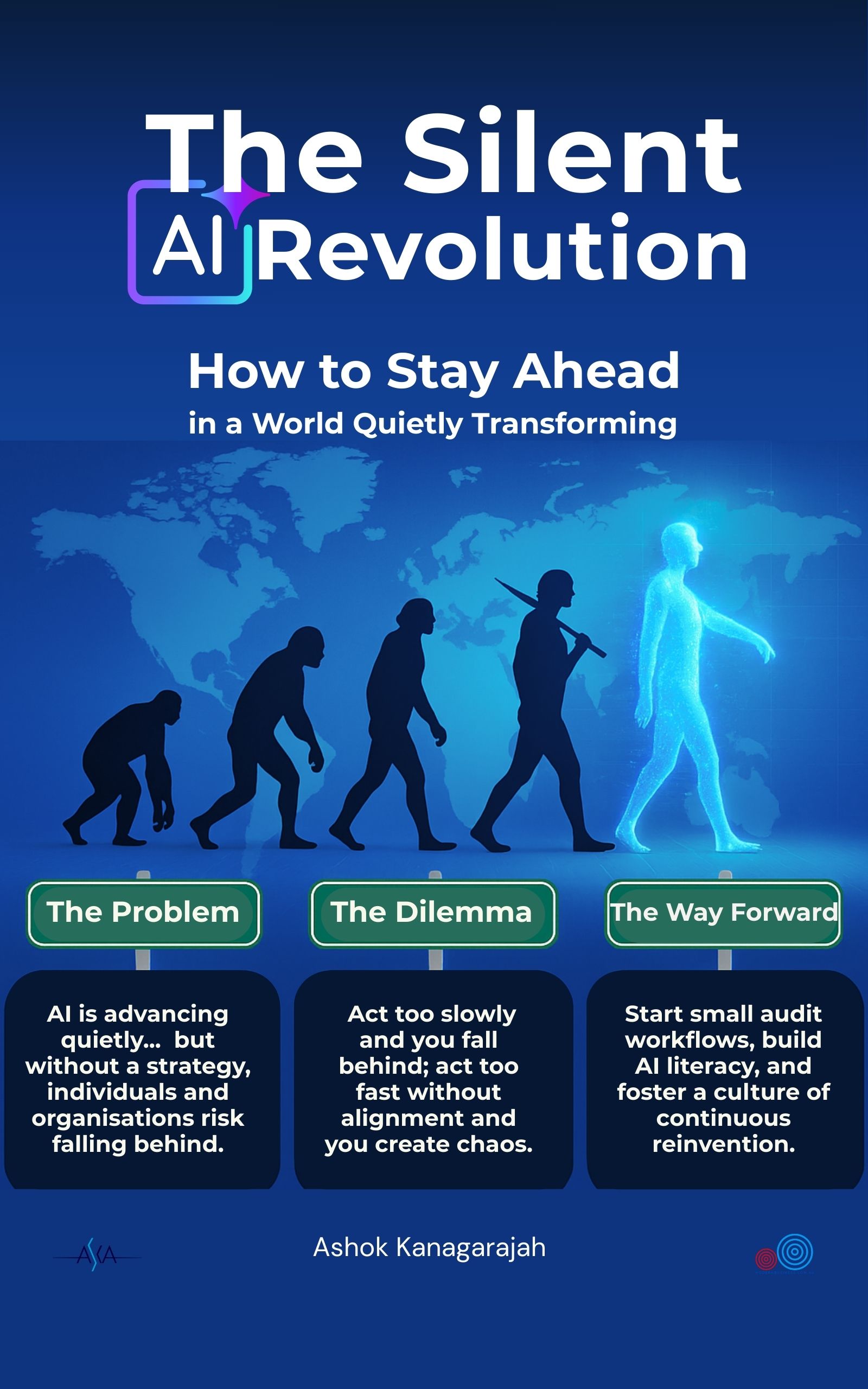
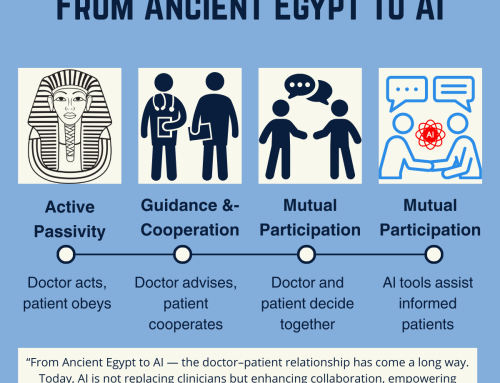
- In Blog 3, we traced the history of the doctor–patient relationship, from ancient Egypt’s activity–passivity model to today’s mutual participation.
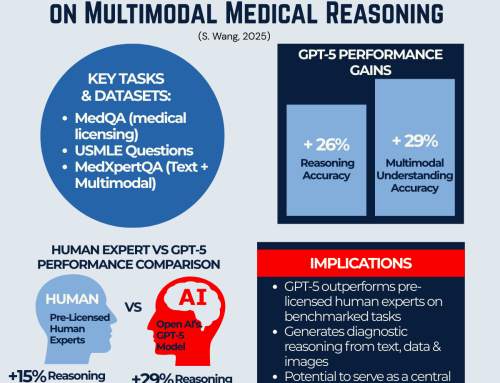
- In Blog 4, we reviewed new evidence from GPT-5 research showing AI models reasoning across text and images at a level comparable to, or beyond, pre-licensed human experts.
Together, these stories form a larger narrative about how healthcare communication between the provider and the patient is being reshaped today.
Hierarchy and Control
For most of history, medicine was defined by hierarchy. In ancient Egypt and well into the modern era, doctors acted as gatekeepers of knowledge, often blending medicine with religion or authority. Patients obeyed. Healthcare was directive, not collaborative.
This was what Kaba and Sooriakumaran later described as the activity–passivity model: the doctor acts, and the patient complies. (Blog 3)
The Patient’s Passive Role
Even as medicine advanced, the relationship often remained unequal. Technical jargon, time pressures, and entrenched hierarchies left patients struggling to understand their care.
Doctors worked hard to help, but patients were still positioned as passive recipients who usually wait for instructions, and rarely actively participate fully in decision-making.
go to: | Start | Top of This Section | End
Carolina’s Case
Carolina’s case showcases a new turning point, enabled by tools like ChatGPT (AI). When she received a biopsy report she couldn’t understand, her doctor wasn’t available, and fear set in. Instead of waiting in panic, Carolina turned to AI. Within minutes, the report was translated into plain language. This didn’t replace her doctor, but it prepared her to ask informed questions and engage in the next consultation with confidence.
Carolina’s Case: A New Kind of Relationship
Because she could understand, Carolina asked better questions.
Because she asked better questions, her doctors could engage at a deeper level.
Because her knowledge matched their explanations, decisions became a partnership.
This is the power of information parity: when patients and clinicians start from the same foundation, conversations become more collaborative, efficient, and empathetic.
The Five Dimensions of patient-centred care (Blog 2) — biopsychosocial perspective, patient-as-person, sharing power, therapeutic alliance, and doctor-as-person — came alive in Carolina’s journey.
And as shown in GPT-5’s research benchmarks, (Blog 4) this isn’t an isolated case. AI can now support reasoning across text, images, and multimodal data, making this kind of partnership possible at scale.
go to: | Start | Top of This Section | End
The Fastest Leap in History
For most of history, shifts in the doctor–patient relationship happened over centuries. Today, AI is accelerating the leap in real time.
Carolina’s story is not just about one patient — it signals a broader transformation. Patients and doctors now have the potential to share the same high-quality reasoning, turning the consultation into a space for decision-making, not just information transfer.
This is the fastest leap in the history of the doctor–patient relationship.
Connecting the Dots
Carolina’s case (Blog 1), the Five Dimensions of care (Blog 2), the historical trajectory (Blog 3), and GPT-5 research (Blog 4) each told part of the story. Together, they point to a fundamental change: healthcare is no longer a one-way street of information delivery — it is a partnership-by-design model.
Doctors remain the essential experts, but their role can expand beyond information delivery to become guides, strategists, and advocates. Patients, equipped with accessible knowledge, can shift from passive recipients to active participants.
The result? Better questions, better conversations, and potentially better outcomes.
go to: | Start | Top of This Section | End
The Now What: Looking Ahead to Blog 6
This story brings us to an important inflection point. The question is no longer if AI will change the doctor–patient conversation, but how we design these conversations for the best outcomes.
The next article in this series will introduce the Patient Journey Communications Framework. It is a practical model that shows how communication flows between patients, doctors, and AI at each stage of care. Understanding these stages will help to apply changes to the existing care models.
Because of its value, this guide (Blog 6) will be available exclusively (but still free) through our membership portal. This ensures it reaches those who are serious about shaping the future of healthcare, not just those curious about AI hype.
go to: | Start | Top of This Section | End
Before you move on, we’d love to hear from you:
- Do you see AI creating information parity in your practice or industry?
- What opportunities or risks do you see if patients and doctors share the same level of reasoning support?
- How might you prepare your organisation to adopt AI responsibly in communication and care?
💬 Your feedback will help refine this series and ensure it delivers maximum value for practitioners, innovators, and healthcare leaders. Please share your thoughts below.
Join the Movement
If this series of blogs has sparked your imagination about how healthcare delivery could be transformed — making it more accessible, affordable, and equitable while also reducing burnout among healthcare professionals — we invite you to connect with the Co-Create Care Movement.
This growing community brings together healthcare innovators, leaders, clinicians, and forward-thinkers who are exploring how AI can be used responsibly to empower patients, support clinicians, and improve outcomes.
Connect with Co-Create Care movement.
→ Facebook Group: Aligning for Excellence
→ Community Link – Meetup Discussions @ AI in Practice (Our Fortnightly Online forum for live discussions)
Together, we can shape a future where healthcare isn’t just sustainable—it’s remarkable.
go to: | Start | Top of This Section | End




Leave A Comment